Families don't start their search for memory care with a brochure. It starts at the dining table in the kitchen, typically in the aftermath of a frightening incident. The father is lost on the way back home from a barbershop. A mother leaves a pot in the kitchen and then forgets it's burning. A spouse wanders after 2 a.m. and activates the house alarm. By the time someone says we require help, the household is already overloaded with the adrenaline and shame. A good assisted living community with dedicated memory care can reset that story. It won't cure dementia, but it can restore safety, routine, and a livable rhythm for everyone involved.
What memory care actually is -- and isn't
Memory care is a specialized model within the broader world of senior living. It's not an unlocked ward in a hospital, and it isn't a house health worker for only the duration of a couple of hours. It sits in the middle and is designed to accommodate people living with Alzheimer's disease, cardiovascular dementia Lewy body dementia, frontotemporal dementia, or mixed causes of cognitive decline. The aim is to reduce risks, maximize remaining abilities, and support a person's identity even as memory changes.
In real terms, this is smaller, more organized environments than typical assisted living, with trained staff on duty around the clock. These neighborhoods are designed for individuals who are prone to forgetting instructions five minutes after hearing them, who may think that a crowded hallway is an attack, or might be perfectly adept at dressing but are unable to manage the steps in a reliable manner. Memory care reframes success: instead of chasing independence as the sole goal, it protects dignity and creates meaningful moments inside a realistic level of support.
Assisted living without a memory care program can still serve residents with mild cognitive issues, especially those who are physically robust and socially engaged. The tipping point tends to arrive when safety demands predictable supervision or when behavioral symptoms, like sundowning, elopement risk, or significant agitation, exceed what a traditional assisted living staff and layout can safely handle.
The layered needs behind cognitive change
Cognitive challenges rarely arrive alone. There is a person who was named Sara who was a teacher retired with Alzheimer's early on who went into assisted living assisted living at her daughter's insistence. She could chat warmly and remember names during the morning but then lapse in the afternoon and claim the staff moved her purse. Her needs on paper seemed to be minimal. In reality they ebbed, flowed, and spiked at odd hours.
Three layers tend to matter the most:
- Brain health and behavior. Memory loss is just one aspect of the picture. It is also evident that there is impaired judgement and executive dysfunction as well as sensory issues, along with sometimes, a rapid change in mood. The best care plans adapt to these shifts hour by hour, not just month by month. Physical wellness. Intoxication may cause confusion. Hearing loss can look like inattention. Constipation can trigger agitation. When a resident suddenly declines cognitively, a seasoned nurse first checks blood pressure, hydration, pain, infection signs, and medication interactions before assuming it's disease progression. Social and environmental fit. People with cognitive impairment mirror the energy around them. A chaotic dining room will amplify anxiety. A familiar routine, a calm tone, and recognizable cues can lower anxiety without a single pill.
Inside strong memory care, these layers are treated as interconnected. Safety measures aren't just door locks. They include hydration schedules, hearing aid checks, soothing lighting, and staff attuned to nonverbal cues that signal discomfort.
What an ordinary day looks like when it's done well
If you tour a memory care neighborhood, don't just ask about philosophy. Watch the rhythms. An early morning may begin with slow, respectful wake-up support rather than busy schedules. The bathroom is provided in the manner that the residents historically preferred, and with options, since control is a primary hazard of routines that are institutionalized. Breakfast includes finger foods for someone who struggles with utensils, and pureed textures for the person at aspiration risk, all plated attractively to preserve appetite.
Mid-morning, the life enrichment team might run a music session featuring songs from the resident's young adulthood. That isn't nostalgia for its own sake. Familiar music lights up brain networks that are otherwise still, and often improves your mood as well as speech throughout the hour that follows. Between, you'll notice short, purposeful tasks: folding towels and watering plants, putting out napkins. They aren't all busywork. They reconnect motor memory to the identity. A retired farmer will respond differently to sorting clothespins than to crafts, and a strong program will adjust accordingly.
Afternoons tend to be the danger zone for sundowning. The most effective is to dim overhead lights, lower ambient noise, provide warm drinks, and shift from cognitively demanding actions to more calm. A structured walk around a secured courtyard doubles as movement therapy and a way to prevent restlessness from turning into exits.

Evenings focus on gentle routines. The beds are lowered early for those who tire following eating dinner. Others may need a late snack to stabilize blood sugar and decrease night-time wandering. Medication passes are paced with conversation rather than rushed, and everyone who needs assisted living it has a toileting prompt before sleep to limit fall risk on nighttime trips to the bathroom.
None of this is fancy. It's straightforward, consistent and repeatable across staff shifts. That is what makes it sustainable.
Design choices that matter more than the brochure photos
Families often react to decor. It's natural. But for memory care, certain design elements quietly determine outcomes far more than a chandelier ever will.
Small-scale neighborhoods lower anxiety. A resident count of 12 to 20 per unit allows staff to know life histories and notice early changes. Oversized, hotel-like floors are harder to supervise and disorienting to navigate.
Circular walking paths prevent dead ends that trigger frustration. Residents who are able to stroll without crashing into a locked door or the cul-de-sac, will experience less exit-seeking incidents. When the path includes a garden or a sunroom, it also helps regulate circadian rhythms.
Contrast and cueing beat clutter. The dark table and the black plate are obliterated by low-contrast eyes. Clear contrasts between plates, placemats, and table surfaces increase food intake. Large, high-contrast signage with icons, such as a simple toilet symbol, helps with wayfinding when words fail.
Residential cues anchor identity. Shadow boxes in every home with photographs and other mementos make hallways personal timelines. An office with a roll-top within a common space can draw a retired bookkeeper into an organizing task. A pretend baby nursery can soothe someone whose maternal instincts are dominant late in life, provided staff supervise and avoid infantilizing language.
Noise control is non-negotiable. Hard floors and TV blaring in open spaces sow the seeds of agitation. Sound-absorbing materials, smaller dining rooms, and TVs with headphone options keep the environment humane for brains that cannot filter stimulus.
Staffing, training, and the difference between a good and a great program
Headcount tells only part of the story. I've witnessed calm active units with an efficient team since every person knew their residents deeply. I have also seen units with higher ratios feel chaotic because staff were task-driven and siloed.
What you want to see and hear:
- Consistent assignments. Aides from the same group work with the same residents over months. Familiar faces read subtle behavioral cues faster than floaters do. Training that goes beyond a one-time dementia module. Be sure to look for continuing education in validation therapy, redirection methods, trauma-informed treatment and non-pharmacological pain evaluation. Ask how often role-play and de-escalation practice occur. A nurse who knows the "why" behind each behavior. Agitation around 4 p.m. could be due to in the form of untreated pain, constipation or a frightened look. A nurse who starts with hypotheses other than "they're sundowning" will spare your loved one unnecessary medication. Real interdisciplinary collaboration. The best programs have the nursing department, activities and housekeeping all in the same room. If the dietary team knows the fact that Mrs. J. reliably eats better after music and they know when she eats, they can plan her meal to suit. That kind of coordination is worth more than a new paint job. Respect for the person's biography. The stories of life should be included to the charts and everyday routine. A retired machinist can handle and sort safe hardware components in 20 minutes of pride. That is therapy disguised as dignity.
Medication use: where judgment matters most
Antipsychotics and sedatives can take the edge off dangerous agitation, but they come with trade-offs: higher fall risk, increased confusion, and in the case of antipsychotics, black box warnings in dementia. An effective memory care program follows a structure. First remove triggers: noise, glare, constipation, infection, hunger, boredom. Try non-pharmacological approaches like aromatherapy, music, massage, exercise, routine modifications. When medications are necessary, the goal is the lowest effective dose, reviewed frequently, with a clear target symptom and a plan to taper.
Families can help by documenting what worked at home. If Dad was calm with a warm washcloth on his neck or with gospel music, it is useful data. Additionally, you can share your past bad reactions even if they occurred the past. Brains with dementia are less forgiving of side effects.
When assisted living is enough, and when a higher level is needed
Assisted living memory care suits people who need 24-hour supervision, cueing with activities of daily living, and structured therapeutic engagement, yet do not require continuous skilled nursing. The resident who needs help with dressing, medication management, and meal support, who occasionally becomes agitated but responds to redirection, fits well.
Signs that a skilled nursing facility or geriatric psychiatry unit may be more appropriate include complex medical equipment, frequent uncontrolled seizures, stage 3 or 4 pressure injuries, intravenous therapies, or severe, persistent aggression that endangers others despite strong non-pharmacological strategies. Some assisted living communities can bridge short-term spikes through respite care or hospice partnerships, but long-term safety drives placement decisions.
The role of respite care for families on the edge
Caregivers often resist the idea of respite care because they equate it with failure. I have watched respite, employed strategically, help preserve families and prolong permanently locating for months. A two-week stay after a hospitalization lets wound care rehabilitation, medication, and stabilization happen within a safe and controlled environment. The four-day break while the primary caregiver attends work prevents crises at home. For many communities, respite can also serve as a test time. The staff learn about the patterns of the resident while the resident gets to know how to live in the community, and then families learn what care really means. When a permanent move becomes necessary, the path feels less abrupt.
Paying for memory care without losing the plot
The arithmetic is sobering. In several regions, charges for monthly memory care inside assisted living run from the mid-$5,000s to over $9,000, depending upon the amount of care provided, the type of room as well as local wage rates. The cost typically covers housing and meals, as well as basic services as well as a base of quality of care. Additional monthly charges are common for higher assistance levels, incontinence supplies, or specialized services.
Medicare does not pay room and board in assisted living. They may also cover services such as nursing, physical therapy visits or hospice care delivered inside the community. Long-term care insurance, when is in effect, will help offset expenses once triggers for benefit are satisfied, typically two or more activities that require daily life or impairment. Veteran spouses and their survivors should ask whether they qualify for their eligibility for the VA Aid and Attendance benefit. Medicaid coverage for assisted living memory care varies by state. Some offer waivers that pay for services, not for rent. Waitlists may be lengthy. Families often braid together sources: private pay, insurance, VA benefits, and eventually Medicaid if available.
One practical tip: ask for a line-item explanation of what is included, what triggers a care-level increase, and how those increases are communicated. Surprises erode trust faster than any care lapse.
How to assess a community beyond the tour script
Sales tours are polished. Real life shows up within the lines. Make sure to visit multiple times, in different time slots. Late afternoon will provide more information about staff ability than the mid-morning craft circle ever could. Bring a simple checklist, then put it away after ten minutes and use your senses.
- Smell and sound. The faint scent of lunch is not unusual. A persistent urine smell could indicate the staffing issue or a system problem. A loud, raucous sound is acceptable. Constant TV blare or chaotic chatter raises red flags. Staff behavior. Monitor interactions, not just numbers. Are staff members kneeling to eye level, use names and provide options? Are they talking to residents, or even about them? Do they notice someone hovering at a doorway and gently redirect? Resident affect. It will show a variety that includes some who are engaged, some asleep, others agitated. What matters is whether engagement is happening in a personalized way, not a one-size-fits-all activity calendar. Safety that doesn't feel like jail. Doors are secure without feeling punitive. Are there outdoor spaces inside the secure perimeter? Are wander management systems discreet and functional? Leadership accessibility. You should ask who will contact you in the event of a problem around 10 p.m. Contact the community at night and check out the reaction. You are buying a system, not just a room.
Bring up tough scenarios. If Mom refuses a shower for 3 days, how will staff respond? If Dad hits another resident What is the order of de-escalation, notification to family members, and care plan change? The best answers are specific, not theoretical.
Partnering with the team once your loved one moves in
The move itself is an emotional cliff. Family members often think that their work has ended, however the initial 30-60 days is when your perspective matters most. Tell a story on one page including photos, your favorite food items and music, as well as hobbies, past work, sleep routines, and triggers that you are aware of. Staff turnover is real in senior care, and a one-page summary travels better than a long binder.
Expect some transitional behaviors. The rate of wandering may increase in the first week. Appetite may dip. Sleep cycles can take time to be reset. Agree on a communication cadence. Check-ins every week with your nursing staff or the care manager are reasonable early on. Find out how any changes to the care level are determined and documented. If a new charge appears on the bill, connect it to a care plan update.
Do not underestimate the value of your presence. A few visits from time on, at varying times will help you understand the true day-to-day rhythm and allow your loved ones to stay connected to their loved ones. If your visits seem to trigger distress, try timing them around favorite activities, shorten the duration, or step back for a few days and confer with the team.
The edges: when things don't go as planned
Not every admission fits smoothly. If a person is suffering from untreated sleep apnea can spiral into daytime anxiety and then nighttime wandering. Getting a new CPAP setup inside respite care assisted living can be surprisingly complex, involving suppliers of medical devices that are durable prescribing, staff, and purchase. Meanwhile, falls may increase. That's where a savvy community to show their metal. They convene an interdisciplinary huddle, loop in the primary care provider, adjust the sleep routine, and escalate carefully to medical interventions.
Or consider a resident whose lifelong stoicism masks pain. The resident becomes angry and aggressive with care. An inexperienced team might increase antipsychotics. A skilled nurse requests the pain test, records behaviors in relation to the dosing, and discovers that scheduled Acetaminophen for breakfast and dinner reduces the severity of symptoms. The behavior wasn't "just dementia." It was a solvable problem.
Families can advocate without becoming adversaries. Focus on results and observations. Instead of blaming others, consider, I've noticed Mom has been refusing to eat the lunch menu three days a week, and her weight is dropping by 2 pounds. Can we review her meal setup, texture, and the dining room environment?
Where respite care fits into longer-term planning
Even after a successful move, respite remains a useful tool. If the resident develops a temporary need that stretches an memory care unit's scope, like intensive wound care A short shift to a skilled setting can be a stabilizing option without giving up the resident's apartment. If families are unsure of an eventual placement in a permanent setting, a 30-day break can be used as a testing period. Staff learn habits as the resident gets used to it, and families can see if the program promised will benefit the loved ones. There are some communities that offer programs for daytime which function as micro-respite. For caregivers still supporting a spouse at home, one or two days per week can extend the workable timeline and keep the marriage intact.
The human core: preserving personhood through change
Dementia shrinks memory, not meaning. The job of memory care inside assisted living is to help keep meaning in grasp. This could mean a retired pastor leading a short blessing before the meal, a woman at home making warm towels fresh from the dryer, or a lifetime dancer dancing at Sinatra in the sunroom. These are not extras. They are the scaffolding of identity.
I think of Robert, an engineer who built model airplanes in retirement. At the point he had to go into memory care, he could not follow complex instructions. The staff provided him with sandpaper, balsa wood scraps, and a simple template, then worked side by side on repetitive motions. His hands glowed when he remember what his brain could not. He wasn't required to complete an airplane. He needed to feel like the man who once did.
This is the difference between elderly care as a set of tasks and senior care as a relationship. A reputable senior living community will know what the difference is. When it happens, families sleep again. Not because the disease has changed, but because the support has.
Practical starting points for families evaluating options
Use this short, focused checklist during visits and calls. It keeps attention on what predicts quality, not just what photographs well.
- Ask for staff turnover rates for aides and nurses over the past 12 months, and how the community stabilizes teams. Request two sample care plans, with resident names redacted, to see how goals and interventions are written. Observe a mealtime. Note plate contrast, staff engagement, and whether assistance preserves dignity. Confirm training frequency and topics specific to memory care, including de-escalation and pain recognition. Clarify how the community coordinates with outside providers: hospice, therapy, primary care, and emergency transport.
Final thoughts for a long journey
Memory care inside assisted living is not a single product. It's a combination of routines, environments, training, and values. It helps seniors facing cognitive challenges by wrapping skilled observation into daily routines and then altering the wrapping as needs evolve. Families who approach the program with calm eyes and constant questions tend to find organizations that are more than close a door. They keep a life open, within the limits of a changing brain.
If you carry anything best respite care forward, make it this: behavior is communication, routines are medicine, and personhood is the north star. Choose the place that behaves as if all three are true.
Business Name: BeeHive Homes Assisted Living
Address: 16220 West Rd, Houston, TX 77095
Phone: (832) 906-6460
BeeHive Homes Assisted Living
BeeHive Homes Assisted Living of Cypress offers assisted living and memory care services in a warm, comfortable, and residential setting. Our care philosophy focuses on personalized support, safety, dignity, and building meaningful connections for each resident. Welcoming new residents from the Cypress and surround Houston TX community.
16220 West Rd, Houston, TX 77095
Business Hours
Monday thru Sunday: 7:00am - 7:00pm
Facebook: https://www.facebook.com/BeeHiveHomesCypress
BeeHive Homes Assisted Living is an Assisted Living Facility
BeeHive Homes Assisted Living is an Assisted Living Home
BeeHive Homes Assisted Living is located in Cypress, Texas
BeeHive Homes Assisted Living is located Northwest Houston, Texas
BeeHive Homes Assisted Living offers Memory Care Services
BeeHive Homes Assisted Living offers Respite Care (short-term stays)
BeeHive Homes Assisted Living provides Private Bedrooms with Private Bathrooms for their senior residents
BeeHive Homes Assisted Living provides 24-Hour Staffing
BeeHive Homes Assisted Living serves Seniors needing Assistance with Activities of Daily Living
BeeHive Homes Assisted Living includes Home-Cooked Meals Dietitian-Approved
BeeHive Homes Assisted Living includes Daily Housekeeping & Laundry Services
BeeHive Homes Assisted Living features Private Garden and Green House
BeeHive Homes Assisted Living has a Hair/Nail Salon on-site
BeeHive Homes Assisted Living has a phone number of (832) 906-6460
BeeHive Homes Assisted Living has an address of 16220 West Road, Houston, TX 77095
BeeHive Homes Assisted Living has website https://beehivehomes.com/locations/cypress
BeeHive Homes Assisted Living has Google Maps listing https://maps.app.goo.gl/G6LUPpVYiH79GEtf8
BeeHive Homes Assisted Living has Facebook page https://www.facebook.com/BeeHiveHomesCypress
BeeHive Homes Assisted Living is part of the brand BeeHive Homes
BeeHive Homes Assisted Living focuses on Smaller, Home-Style Senior Residential Setting
BeeHive Homes Assisted Living has care philosophy of “The Next Best Place to Home”
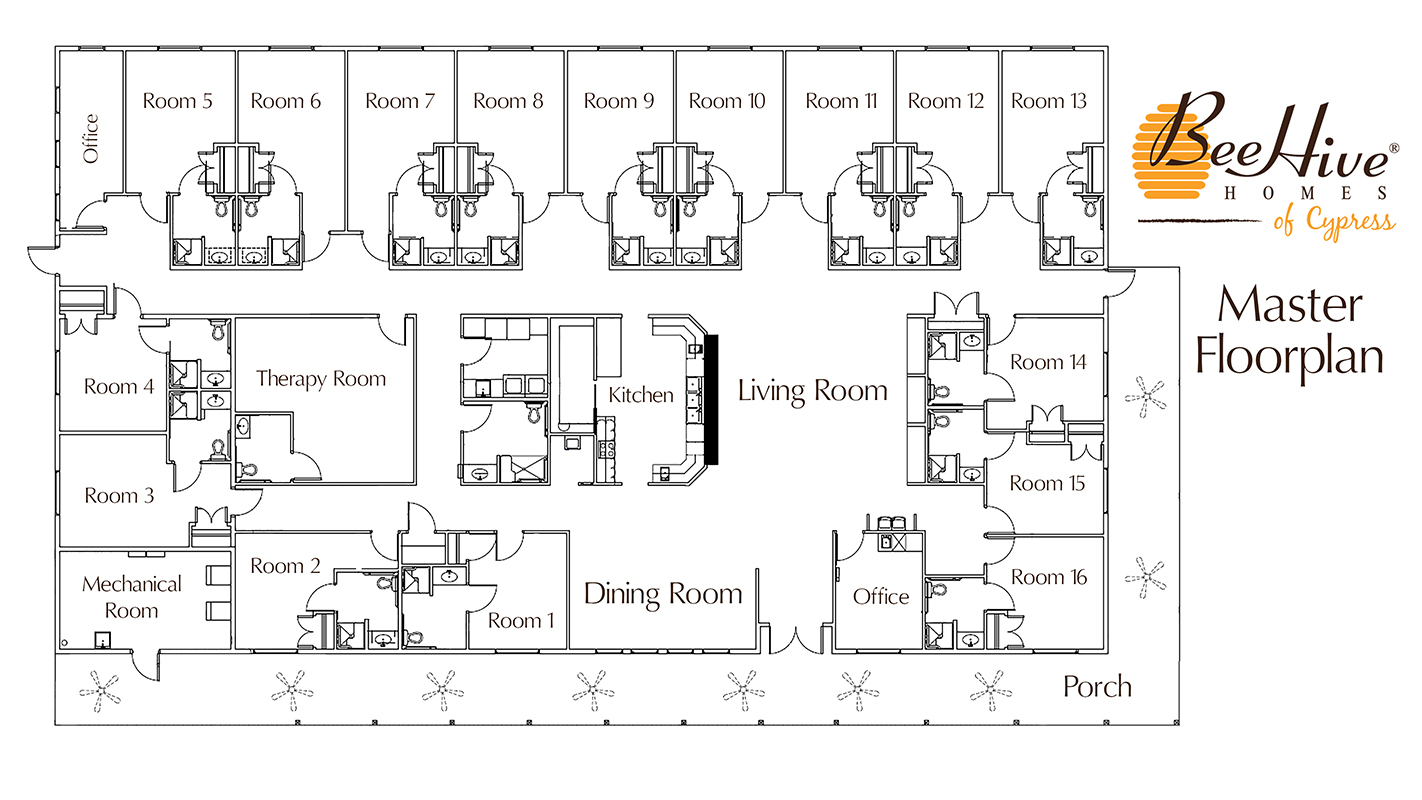
BeeHive Homes Assisted Living has floorplan of 16 Private Bedrooms with ADA-Compliant Bathrooms
BeeHive Homes Assisted Living welcomes Families for Tours & Consultations
BeeHive Homes Assisted Living promotes Engaging Activities for Senior Residents
BeeHive Homes Assisted Living emphasizes Personalized Care Plans for each Resident
People Also Ask about BeeHive Homes Assisted Living
What services does BeeHive Homes of Cypress provide?
BeeHive Homes of Cypress provides a full range of assisted living and memory care services tailored to the needs of seniors. Residents receive help with daily activities such as bathing, dressing, grooming, medication management, and mobility support. The community also offers home-cooked meals, housekeeping, laundry services, and engaging daily activities designed to promote social interaction and cognitive stimulation. For individuals needing specialized support, the secure memory care environment provides additional safety and supervision.How is BeeHive Homes of Cypress different from larger assisted living facilities?
BeeHive Homes of Cypress stands out for its small-home model, offering a more intimate and personalized environment compared to larger assisted living facilities. With 16 residents, caregivers develop deeper relationships with each individual, leading to personalized attention and higher consistency of care. This residential setting feels more like a real home than a large institution, creating a warm, comfortable atmosphere that helps seniors feel safe, connected, and truly cared for.Does BeeHive Homes of Cypress offer private rooms?
Yes, BeeHive Homes of Cypress offers private bedrooms with private or ADA-accessible bathrooms for every resident. These rooms allow individuals to maintain dignity, independence, and personal comfort while still having 24-hour access to caregiver support. Private rooms help create a calmer environment, reduce stress for residents with memory challenges, and allow families to personalize the space with familiar belongings to create a “home-within-a-home” feeling.Where is BeeHive Homes Assisted Living located?
BeeHive Homes Assisted Living is conveniently located at 16220 West Road, Houston, TX 77095. You can easily find direction on Google Maps or visit their home during business hours, Monday through Sunday from 7am to 7pm.How can I contact BeeHive Homes Assisted Living?
You can contact BeeHive Assisted Living by phone at: 832-906-6460, visit their website at https://beehivehomes.com/locations/cypress/,or connect on social media via Facebook
BeeHive Assisted Living is proud to be located in the greater Northwest Houston area, serving seniors in Cypress and all surrounding communities, including those living in Aberdeen Green, Copperfield Place, Copper Village, Copper Grove, Northglen, Satsuma, Mill Ridge North and other communities of Northwest Houston.